Edinburgh mum-of-three sheds light on '˜death sentence' anorexia battle
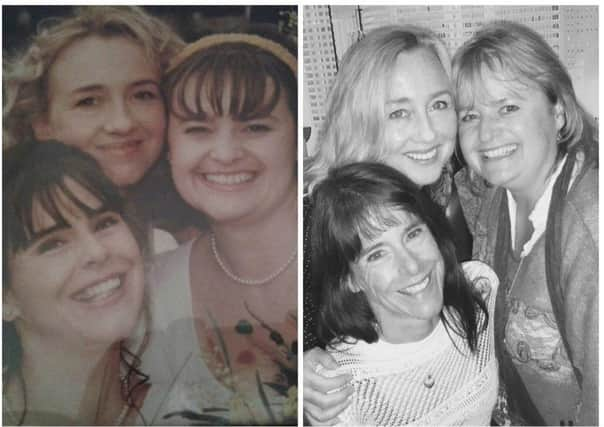

Wendy Robbins’ 20-year battle with anorexia has left her an emaciated five stone and in a fight for her life.
And although she backs the NHS and the support she gets, the 50-year-old has called for more tailored services for those facing a similar plight.
Advertisement
Hide AdAdvertisement
Hide AdWendy, from Edinburgh, said: “It’s a death sentence. It’s a very real illness and extremely difficult for people to understand.


“It’s difficult to love someone and watch them and stay with them – it’s by far the biggest killer of mental health related illnesses.”
Wendy was admitted to the Regional Eating Disorder Unit at Livingston’s St John’s Hospital in January but her stay was cut short after she was found hiding food in a napkin.
Her potassium levels had dropped to such drastic levels, staff at the centre grew suspicious.
Advertisement
Hide AdAdvertisement
Hide AdShe maintained she gets “fantastic support” from the NHS but questioned the method of treatment.


“My main concern is it’s very much geared to feeding people up, making them stable and sending them home again – it’s putting a plaster over a festering wound.”
Wendy is now considering private treatment in one last throw of the dice – but it could mean selling her home.
“I’m not looking for a fundraising campaign from the public, that’s not what I’m after. I don’t want pity. I could borrow money or if I need to, I can sell my house.
Advertisement
Hide AdAdvertisement
Hide Ad“There’s a serious lack of eating disorder services available. Almost all, if not all, are rehabilitation for addictions.”
One option currently unavailable is to emigrate to South Africa where treatment is more “holistic” as her Body Mass Index is currently too low.
“I could go into the Priory and get weight on and then go out there,” she added.
One of the toughest casualties of Wendy’s condition to bear is the impact on her lifelong interest in exercise – a passion she shares with her three children – twins, aged 20, and a 15-year-old.
Advertisement
Hide AdAdvertisement
Hide Ad“The last time I ran was at Christmas,” she said. “I haven’t been swimming either. I’ve swum all my life but it’s too cold in the pool.
“I can’t face going into the water. I get out of breath. It’s as natural to me as cleaning my teeth – I’ve always been very active.”
Another dream relinquished is a lifelong ambition to volunteer in Africa – a continent she built an “affinity” with since childhood.
“I feel very sad because I’ve always been an advocate of the NHS and I think we’re incredibly lucky in the UK and particularly in Scotland.
Advertisement
Hide AdAdvertisement
Hide Ad“I just feel really disappointed and quite down that the mental health side of illness is a juggernaut that is just taking its time.
“There seem to be these anomalies that they wouldn’t send a cancer patient home if they were terminally ill, saying they couldn’t treat them – they’d provide ongoing care and support.
“I feel very let down. This is my hope – even if it doesn’t help in my position – in the future there are the services there.”
Wendy said her experience made it obvious more support is needed for suicidal patients and those with eating disorders.
Advertisement
Hide AdAdvertisement
Hide Ad“I would like to see much more funding going in – patient care for people with severe mental health issues.”
Wendy’s plight has been taken up by her MSP Gordon Macdonald who wrote to NHS Lothian chief executive Tim Davison on her behalf and is awaiting a response.
“Wendy is in an extremely vulnerable situation and I am disappointed that she is not receiving the help that she desperately requires,” said Mr Macdonald.
“I have been supporting her as much as I possibly can and have raised Wendy’s case with NHS Lothian on a number of occasions and, last week, escalated it to the Chief Executive as a matter of urgency – I expect NHS Lothian to take swift action to get Wendy the vital help she needs and to ensure that lessons are learned for the future.”
Advertisement
Hide AdAdvertisement
Hide AdMr Macdonald called for the same focus and action on mental health illness as physical ailments.
“The seriousness of eating disorders and the impact on sufferers, their families and their friends is clear,” he said.
“Health professionals must look at the whole person when someone presents with an eating disorder.
“The Scottish Government’s guiding ambition of their mental health strategy is that someone should only have to “ask once, get help fast”, and that we must prevent and treat mental health problems with the same commitment, passion and drive as we do physical health problems.
Advertisement
Hide AdAdvertisement
Hide Ad“We must do all that we can to make sure that this ambition is the reality, for those that need it most.”
NHS Lothian’s Director of Nursing, Professor Alex McMahon, praised the work of the Regional Eating Disorder Unit at St John’s Hospital.
“We cannot comment on individual cases without the consent of the patient involved,” said Prof McMahon.
“The Regional Eating Disorders Unit is a specialist facility for patients from all over the south east of Scotland.
Advertisement
Hide AdAdvertisement
Hide Ad“The expert clinical teams develop personalised short or longer term treatment plans for every patient which are agreed in advance.
“We know the pressures that a specialist inpatient unit can hold and we are aware that patients can take a break and return at a later date, which is why we arrange specialist outpatient treatment and support with other clinical teams.”